
ريزوم العلاج ببخار الماء
هل يجب أن أفكر في العلاج بالطرق الأقل تدخلاً؟
مع تقدم الرجال في السن، تتضخم غدة البروستاتا بشكل طبيعي، مما يؤدي إلى أعراض بولية وعدم راحة.
تقليديا، كانت خيارات العلاج لتضخم البروستاتا الحميد تقتصر في كثير من الأحيان على الجراحة أو الأدوية، ولكن التطورات الأخيرة في التكنولوجيا الطبية فتحت الباب لخيارات علاج أقل تدخلاً ولكنها فعالة للغاية.
في هذه المقالة، سوف نستكشف العلاجات الجراحية قليلة التدخل، والمعروفة باسم MIST، لمساعدتك في الإجابة على سؤال شائع جدًا - هل يجب أن تفكر في الحصول على علاج قليل التدخل لتخفيف أعراض تضخم البروستاتا الحميد؟
ما هو MIST؟
أولاً، دعونا نبدأ بتوضيح ما هو العلاج الجراحي بالحد الأدنى من التدخل (MIST). العلاجات الجراحية الأقل توغلاً (MIST) لعلاج تضخم البروستاتا الحميد (BPH) هي إجراءات يمكن إجراؤها بدون تخدير عام أو إقامة في المستشفى.
تتطلب هذه الإجراءات الأقل تدخلاً فترة نقاهة قصيرة، وهي إجراءات للمرضى الخارجيين، ولا تتطلب دائمًا من المرضى ارتداء قسطرة بعد العملية. يتمكن المرضى الذين يخضعون لهذه العلاجات من العودة إلى أنشطتهم اليومية في غضون أيام قليلة بعد العملية.
إنها تخفف أعراض تضخم البروستاتا الحميد لدى المرضى دون استخدام الأدوية أو الغرسات الدائمة، وتسمح للمرضى بتجربة تخفيف الأعراض في غضون أسبوعين.
فوائد العلاجات الأقل تدخلاً
إذن، ما هي فوائد إجراء عملية جراحية طفيفة التوغل؟ حسنًا، هناك العديد من الفوائد، بما في ذلك ما يلي:
- تتطلب هذه الإجراءات فترة نقاهة قصيرة . والفرق الرئيسي بين علاجات MIST وعلاجات تضخم البروستاتا الحميد الأخرى هو أنها قليلة التدخل مع فترة نقاهة قصيرة. ولا يحتاج المرضى إلى قضاء وقت في المستشفى أو أخذ إجازة كبيرة. وبدلاً من ذلك، يمكنهم العودة إلى أنشطتهم المعتادة في غضون يومين.
- تحافظ على الوظيفة الجنسية . يمكن لعلاجات MIST الحفاظ على الوظيفة الجنسية. لا تسبب عمومًا آثارًا جانبية جنسية، ولا تتداخل مع قدرة المرضى على الأداء أثناء الجماع. أفاد المرضى أن هذه العلاجات لا تسبب ضعف الانتصاب أو القذف الذي قد ينشأ مع علاجات تضخم البروستاتا الحميد الأخرى.
- إنها غير جراحية ولا تتطلب أي أدوية . تعمل علاجات MIST على تخفيف أعراض تضخم البروستاتا الحميد بأمان وفعالية، دون الحاجة إلى تناول أي أدوية أو تركيب أي غرسات دائمة. يشعر المرضى عمومًا بتحسن الأعراض في غضون أسبوعين فقط بعد الإجراء.
هل أنا مرشح لبرنامج MIST؟
بعد معرفة المزيد عن هذه الإجراءات، قد تسأل نفسك - هل أنا مرشح لإجراء جراحي أقل تدخلاً؟
حسنًا، عادةً ما تكون علاجات MIST مناسبة للرجال الذين لا يرغبون في تناول أي أدوية لعلاج أعراض تضخم البروستاتا الحميد بشكل مستمر، أو الذين كانت لديهم تجربة سيئة سابقة مع الأدوية. كما يوصى بها للرجال الذين لا يرغبون في الخضوع لمخاطر التدخل الجراحي القياسي.
إذا كان من الممكن الحصول على نتائج علاجية مرضية باستخدام خيار MIST، فهذا هو الخيار المفضل عادةً لتجنب المخاطر والآثار الجانبية للجراحة أو الدواء.

تضخم البروستاتا الحميد: الأساطير مقابل الحقائق
تضخم البروستاتا الحميد: الأساطير مقابل الحقائق
قد يكون من الصعب للغاية التغلب على المفاهيم الخاطئة والشكوك المحيطة بتضخم البروستاتا الحميد. وكحالة شائعة تصيب الرجال، غالبًا ما يجد تضخم البروستاتا الحميد نفسه متورطًا في أساطير يمكن أن تعيق الفهم الدقيق والتدخل في الوقت المناسب.
في هذا المقال، نهدف إلى كشف الحقائق المحيطة بتضخم البروستاتا الحميد، والتمييز بين الأساطير والحقائق. وسنعمل على دحض المفاهيم الخاطئة الشائعة والحصول على فهم أوضح لهذا الجانب من صحة الرجال.
الأسطورة: الإصابة بتضخم البروستاتا الحميد تعني تلقائيًا إصابتك بالسرطان
ربما تكون هذه هي الأسطورة الأكثر شيوعًا التي تنتشر حول موضوع تضخم البروستاتا الحميد. لا، لا يعني وجود تضخم البروستاتا الحميد تلقائيًا إصابتك بالسرطان. في حين أن تضخم البروستاتا الحميد وسرطان البروستاتا يشتركان في بعض الأعراض المتشابهة، إلا أنهما حالتان مختلفتان تمامًا.
تضخم البروستاتا الحميد هو حالة غير سرطانية تحدث عادة لدى الرجال المسنين، وتتضمن تضخم غدة البروستاتا. من ناحية أخرى، فإن سرطان البروستاتا هو نمو خبيث للخلايا في غدة البروستاتا. من المهم عدم استخلاص استنتاجات، حيث أن العديد من الرجال المصابين بتضخم البروستاتا الحميد لا يصابون بسرطان البروستاتا.
الأسطورة: تضخم البروستاتا يسبب أعراضًا أسوأ
مرة أخرى، هذه خرافة. إن كبر حجم البروستاتا لا يعني بالضرورة أنك ستعاني من أعراض أسوأ. وفي حين أن كبر حجم البروستاتا لا يضمن حدوث مشكلات، فإن صغر حجم البروستاتا لا يضمن تجنب العلاج.
عندما يتعلق الأمر بأعراض تضخم البروستاتا الحميد، فإن ما يهم ليس حجم البروستاتا، بل ما يحدث بداخلها. إذا شعر الطبيب بتضخم البروستاتا أثناء الفحص الشرجي، فهذا لا يعني تلقائيًا وجود انسداد بالداخل.
الحقيقة: تضخم البروستاتا الحميد شائع للغاية عند الرجال
نعم، صحيح أن تضخم البروستاتا الحميد هو حالة شائعة بين الرجال، وخاصة مع تقدمهم في السن. حيث يتضخم حجم البروستاتا بشكل طبيعي مع تقدم الرجال في السن، وقد يؤدي هذا التضخم إلى ظهور أعراض بولية مختلفة.
في الواقع، يزداد انتشار تضخم البروستاتا الحميد مع تقدم العمر، وتشير التقديرات إلى أن حوالي 50% من الرجال الذين تتراوح أعمارهم بين 51 و60 عامًا يعانون من درجة ما من تضخم البروستاتا. وبحلول سن الثمانين، قد يعاني حوالي 80% من الرجال من أعراض تضخم البروستاتا الحميد. ورغم أن تضخم البروستاتا الحميد شائع، إلا أن ليس كل الرجال الذين يعانون من تضخم البروستاتا الحميد سيعانون بالضرورة من أعراض كبيرة.
الحقيقة: يمكن أن يسبب تضخم البروستاتا الحميد مشاكل خطيرة أخرى
على الرغم من أن تضخم البروستاتا الحميد لا يعتبر حالة خطيرة أو مهددة للحياة، إلا أنه قد يؤدي إلى مضاعفات ويؤثر على جودة حياة الشخص. يمكن أن يؤدي تضخم البروستاتا الحميد إلى إفراغ المثانة بشكل غير كامل، مما يزيد من خطر الإصابة بعدوى المسالك البولية. بالإضافة إلى ذلك، قد يؤدي عدم القدرة على إفراغ المثانة بالكامل إلى تكوين حصوات المثانة.
في بعض الحالات، قد يؤدي تضخم البروستاتا الحميد إلى عدم القدرة على التبول بشكل مفاجئ وكامل، مما يؤدي إلى حالة طبية طارئة تُعرف باسم احتباس البول الحاد. قد تؤدي الحالات الشديدة من تضخم البروستاتا الحميد، إذا تُركت دون علاج، إلى مشاكل مزمنة في الكلى بسبب احتباس البول وتدفق البول إلى الكلى.
تخلص من حصوات الكلى باستخدام العلاج بالليزر بدون ندبات
تخلص من حصوات الكلى باستخدام العلاج بالليزر بدون ندبات
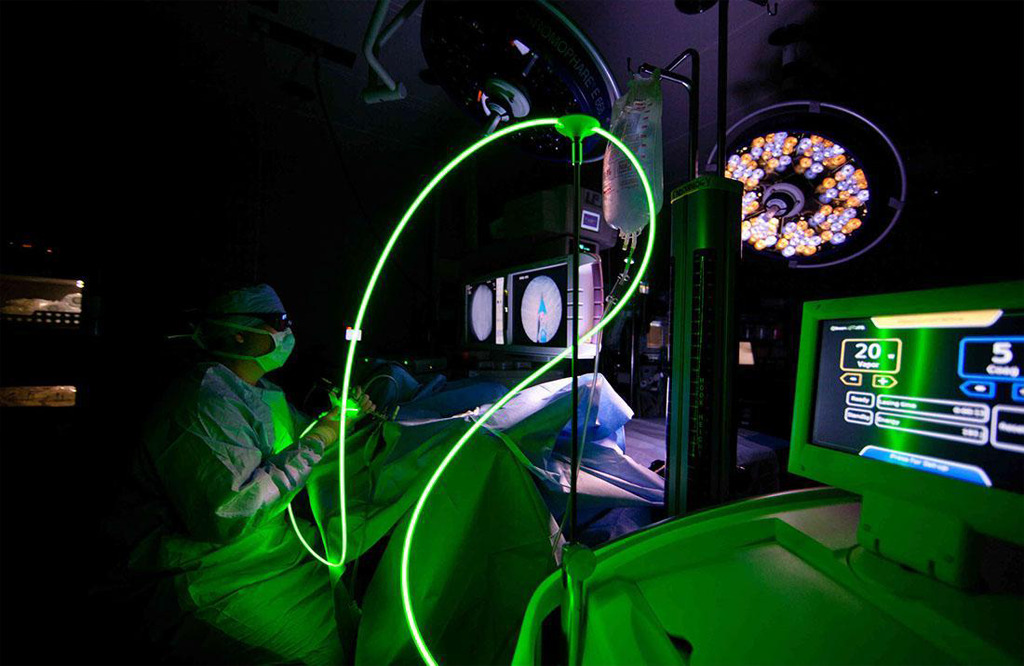
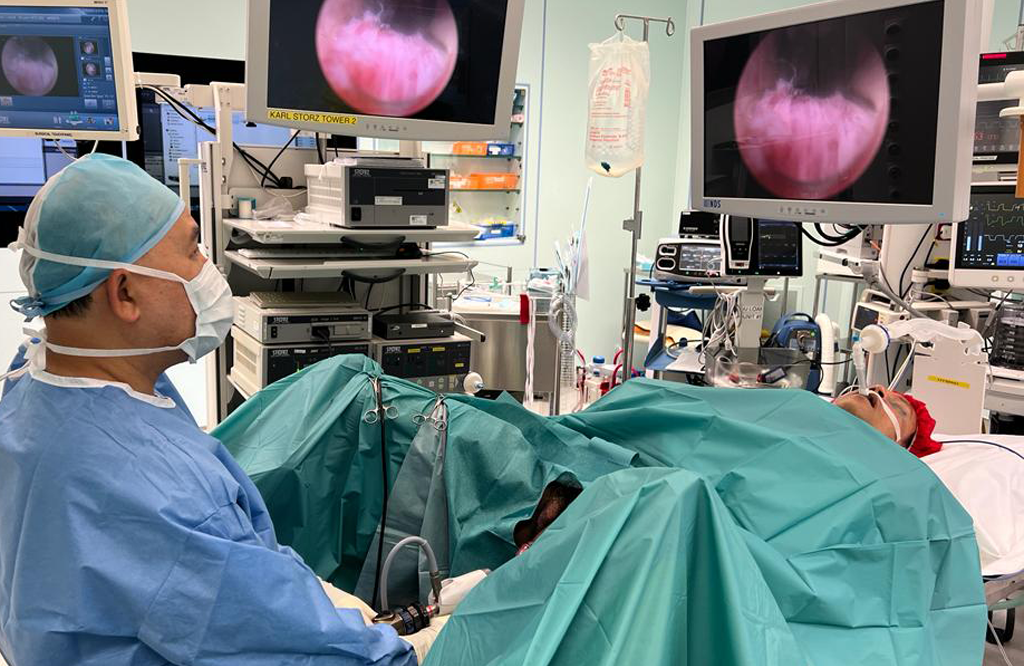
الجراحة الراجعية داخل الكلى (RIRS) هي جراحة بالمنظار يتم إجراؤها لإزالة حصوات الكلى. يتم إجراء العملية باستخدام منظار الحالب المرن، والذي يتم وضعه من خلال مجرى البول (فتحة البول) إلى المثانة ثم من خلال الحالب إلى الكلى (منطقة داخل الكلى). من خلال هذا الجهاز، يتم استخدام ألياف الليزر (ليزر الهولميوم) لعلاج الحصوات.
كيف يتم علاج حصوات الكلى باستخدام نظام RIRS؟
يحتوي منظار الحالب على كاميرا صغيرة مثبتة في نهايته تُستخدم لفحص حصوات الكلى . تعرض شاشة المراقبة الموجودة في غرفة الجراحة التشريح الكامل لكلية المريض الذي تم التقاطه بواسطة منظار الحالب. من خلال موجة الموجات فوق الصوتية أو مسبار الليزر، يتم سحق الحصوات إلى مسحوق ناعم أو قطع. يمكن لهذه القطع الدقيقة أن تمر بسهولة خلال عملية التبول.
ما هي مزايا تقنية RIRS مقارنة بالتقنيات القديمة مثل PCNL (جراحة ثقب المفتاح)؟
إن عملية RIRS أقل تدخلاً بالتأكيد من التقنيات القديمة مثل PCNL أو الجراحة بالمنظار أو الجراحة المفتوحة لأنها لا تترك ندبات على الإطلاق. ولأننا ندخل إلى الكلية من خلال المسالك البولية الطبيعية ولا توجد حاجة إلى إجراء أي جروح على الجلد أو ثقب في الكلية (كما في PCNL)، فإن خطر النزيف الشديد أقل، كما أن الإقامة في المستشفى قصيرة جدًا (جراحة نهارية في معظم الحالات)، وهناك فترة تعافي أقصر بشكل ملحوظ ويمكن للمريض العودة إلى روتينه الطبيعي قريبًا جدًا.
من يمكنه إجراء RIRS؟
يتم إجراء RIRS بواسطة أخصائي أمراض المسالك البولية (أخصائي أمراض المسالك البولية الداخلية) ذو الخبرة الخاصة في RIRS.
ما هي ميزة استخدام الليزر عالي القدرة في RIRS؟
يمكن تحقيق أفضل النتائج للمرضى باستخدام الليزر عالي الطاقة. كما يمكن أيضًا إزالة الحصوات لدى المرضى الذين يعانون من حصوات الكلى التي يصل حجمها إلى 4 سم (حصوات قرن الوعل) فقط باستخدام ليزر هولميوم عالي الطاقة.
هل من الضروري تركيب دعامة بعد عملية استبدال الصمام التاجي؟ وهل هي دعامة دائمة؟
نعم، مثل أي جراحة أخرى لحصوات الكلى، يتم وضع دعامة مزدوجة في الحالب في معظم حالات استئصال حصوات الكلى عن طريق المستقيم. الغرض من دعامة مزدوجة هو إبقاء الحالب مفتوحًا أثناء غسل شظايا الحصوات بالليزر، كما أنها تقلل من خطر تضيق الحالب بعد أي تدخل. لا، يتم الاحتفاظ بدعامة مزدوجة مؤقتًا لمدة 2 إلى 4 أسابيع فقط ثم إزالتها من خلال مجرى البول بالمنظار، وهي عملية قصيرة ويمكن للمريض العودة إلى المنزل في نفس اليوم بعد إزالتها.
هل يمكن استخدام RIRS لعلاج أمراض أخرى غير حصوات الكلى؟
نعم، يمكن استخدام RIRS لعلاج الانسدادات في الحالب (التضيقات/انسداد الوصلة البولية المحيطة بالكليتين)، وأورام الحالب ونظام التجميع (للتشخيص وكذلك العلاج).
إن تقنية RIRS هي مستقبل جراحة الحصوات. فهي تتطلب قدرًا معقولاً من الخبرة لإتقان تقنية RIRS ولكنها مفيدة للغاية للمريض. في مستشفى سارفودايا، لدينا معهد متخصص في جراحة المسالك البولية بالليزر مزود بأحدث التقنيات وجهاز ليزر هولميوم متقدم للغاية لعلاج عدة أنواع من حالات حصوات الكلى المعقدة . يمكن للمريض الذي يأتي إلى المستشفى اليوم بحصوة في الكلى أن يخرج من المستشفى بعد الجراحة في اليوم التالي ويعود إلى العمل قريبًا. يجب على المريض أن يأخذ عددًا أقل من أيام الإجازة من العمل بعد الجراحة.
علاج حصوات الكلى
علاج حصوات الكلى
نظرًا لأن حصوات الكلى مرض شائع، فمن الطبيعي أن نسعى إلى إيجاد علاجات فعالة لهذه الحصوات المزعجة.
بالطبع، هناك العديد من الطرق لعلاج حصوات الكلى. ولا أحد منا يرغب في الشعور بالندم لاحقًا لاختياره الحل "غير الكافي" لأي حالة.
عندما يريد شخص ما التخلص من مشكلة مؤلمة لتجنب المضاعفات اللاحقة، فإن اختيار خيار العلاج المؤلم والخطير المحتمل ليس قرارًا جيدًا.
يجب أن يكون علاج حصوات الكلى الناجح آمنًا وفعالًا. تحقق عملية حصوات الكلى الحالية باستخدام الليزر النتيجة المرجوة.
معنى تفتيت الحصى بالليزر
تُستخدم نبضات الضوء تحت الحمراء القصيرة والقوية في تفتيت الحصى بالليزر. وعند استخدامها بشكل صحيح، تكون هذه النبضات قوية لدرجة أنها قادرة على تفتيت أي نوع من الحصى إلى قطع صغيرة. وتُستخدم نفس الطريقة في تفتيت الحصى بالليزر لإزالة حصى الكلى، حيث يتم تفتيت الحصى الموجودة في الكلى إلى قطع صغيرة وطردها عبر البول.
إنها عملية طبيعية غير مؤلمة، ويمكن للمريض التعافي منها بسرعة على عكس أشكال الجراحة التقليدية والتقليدية التي ليست صعبة فحسب، بل تستغرق وقتًا أيضًا لمساعدة الأشخاص على التعافي.
مميزات تنظير الحالب مقارنة بعلاجات الحصوات الأخرى
- تتميز عملية تنظير الحالب المرن بميزة السماح بالدخول إلى جميع أقسام الكلى إذا كانت حصوات الكلى ذات حجم وموضع مقبولين. وطالما أن الحالب كبير بما يكفي للسماح لمنظار الحالب بالمرور من خلاله، فيمكن تفتيت الحصوة وإزالتها في عملية جراحية واحدة.
- على عكس تفتيت الحصوات بالموجات الصادمة، يمكن رؤية حصوات الكلى أو الحالب مباشرة بواسطة منظار الحالب، مما يسمح بتفتيت الحصوات بالليزر ثم تكديسها وإزالتها. يُطلب من المرضى تمرير جزيئات الحصوات بأنفسهم أثناء تفتيت الحصوات بالموجات الصادمة، مما قد يسبب المزيد من الألم أو الانسداد. علاوة على ذلك، قد لا يؤدي تفتيت الحصوات بالموجات الصادمة إلى تفتيت الحصوات شديدة الكثافة والصلبة (المعروفة باسم الحصوات المقاومة لتفتيت الحصوات بالموجات الصادمة). إذا كانت الحصوة مرئية لمنظار الحالب، فيمكن لفحص الحالب باستخدام ليزر هولميوم التلامسي تفتيتها. علاوة على ذلك، يمكن لفحص الحالب علاج الحصوات غير المرئية بالأشعة السينية القياسية (الحصوات "الحامضية").
- على عكس الإجراءات الجلدية، يتم تمرير منظار الحالب من خلال فتحات الجسم الطبيعية ولا يتطلب أي شقوق في الجلد. إنها عملية جراحية للمرضى الخارجيين، في حين تتطلب عملية تفتيت الحصوات الكلوية بالمنظار البقاء في المستشفى لليلة واحدة على الأقل. يمكن علاج مجموعات معينة من المرضى الذين لا يمكن علاجهم باستخدام تفتيت الحصوات الكلوية بالمنظار (مثل أولئك الذين يتناولون مميعات الدم، والنساء الحوامل، والمصابين بالسمنة المفرطة، والطيارين/رواد الفضاء) بأمان وكفاءة باستخدام منظار الحالب.
الأشياء التي تحدث في يوم الجراحة
قبل علاج حصوات الكلى بالليزر، سينصحك الجراح بكيفية التعامل مع أدويتك وطعامك. معظم علاجات حصوات الكلى بالليزر هي إجراءات خارجية، لذا يمكنك العودة إلى المنزل في نفس اليوم.
سيتم تخديرك أثناء العملية لأنك ستخضع للتخدير العام. وهذا يضمن بقائك ساكنًا أثناء وجود الأدوات الصغيرة داخل جسمك. تعد أجهزة الليزر الحديثة أكثر دقة وقوة، مما يسهل على الجراحين التحكم في الحصوة وتفتيتها. كما أنها تقصر مدة العملية، مما يسمح لك بالنوم بشكل أقل والعودة إلى روتينك اليومي في وقت أقرب.
الشعور بعد الجراحة
بعد جراحة الليزر، قد لا تزال تشعر بالألم. إذا كان لديك دعامة بين الكلية والحالب، فمن المرجح أن تكون الدعامة هي مصدر الألم لأنها يمكن أن تحتك بالكلى أو المثانة. يمكن أن تجعلك أيضًا تشعر بالحاجة إلى التبول، وقد تتسبب في وجود بعض الدم في البول. قد يعاني الرجال أيضًا من ألم في القضيب أو الخصيتين.
بعد الجراحة، سيصف لك طبيبك الأدوية. وقد تشمل هذه الأدوية بشكل عام المضادات الحيوية لمنع العدوى، ومسكنات الألم، والأدوية لتخفيف تقلصات المثانة والحروق أثناء التبول.
اشرب الكثير من الماء للحفاظ على ترطيب الدعامة ومنع دخول أي حصوات صغيرة إلى الكلى. قد تحتاج إلى التبول بشكل متكرر، لذا احرص على وجود حمام قريب.
يمكنك العودة إلى ممارسة أنشطتك الطبيعية في اليوم التالي أو بمجرد أن تشعر بالراحة. يجب تجنب التمارين عالية الكثافة حتى تتم إزالة الدعامة. تمنع بعض مسكنات الألم أنشطة مثل القيادة، لذا اقرأ الملصق بعناية. سيقدم لك طبيبك إرشادات إضافية.
مطلوب متابعة الرعاية
بعد الجراحة، سوف ترى الجراح أو مساعديه بعد حوالي أسبوع. إذا كان لديك دعامة، فسيتم إزالتها باستخدام أداة صغيرة مضاءة في هذه المرحلة (منظار المثانة). يتم ذلك مرة أخرى من خلال المثانة ويمكن القيام به أثناء اليقظة في العيادة. إذا كان الجراح يعتقد أنها ستساعد في الشفاء، فقد يتم ترك الدعامة في مكانها لفترة أطول. يمكن أن تظل الدعامة في مكانها لمدة تصل إلى ثلاثة أشهر، لذلك لا تقلق إذا تأخرت إزالة الدعامة. يجب إزالة الدعامة، لذلك لا تنس جدولة فحص ما بعد الجراحة.
سيقوم الجراح بإرسال إحدى حصوات الكلى للتحليل بعد إزالتها. سينصحك طبيبك بكيفية تجنب حصوات الكلى في المستقبل بناءً على تكوين الحصوات. قد يقدم الطبيب أيضًا توصيات بناءً على تحليل البول. على سبيل المثال، قد ينصحك الطبيب بإجراء تعديلات على نظامك الغذائي أو تناول المكملات الغذائية أو الأدوية.
نظرًا لأن حصوات الكلى حالة مزمنة، فقد تتكرر في وقت ما في المستقبل. أنت الآن تفهم الأعراض وأن العلاجات الفعّالة متاحة. اتبع نصيحة طبيب المسالك البولية الخاص بك للمساعدة في منع حصوات الكلى الإضافية، ولا تتردد في الاتصال إذا عادت الأعراض.
المضاعفات والمخاطر
إن عملية تفتيت حصوات الحالب باستخدام الليزر هي علاج آمن وفعال وسريع التعافي. ونتيجة لذلك، لا توجد مخاطر أو صعوبات مرتبطة بالعملية. ومع ذلك، تشمل الآثار الجانبية غير العادية الغثيان وفترة قصيرة من النزيف.
خاتمة
من المؤكد أن حصوات الكلى يمكن أن تكون مؤلمة للغاية وتجعل حياتك بائسة. يستغرق علاجها بالعلاجات القياسية وقتًا طويلاً، كما أن التعافي منها يكون بطيئًا أيضًا. لحسن الحظ، يمكننا الآن علاج حصوات الكلى بالمنظار البولي وتفتيت الحصى بالليزر. المخاطر طفيفة، ويشفى المريض بسرعة دون آثار جانبية كبيرة. العلاج بالكامل خالٍ من المخاطر ويستغرق من 10 دقائق إلى ساعة، اعتمادًا على شدة العملية.
إذا كنت تعاني من حصوات الكلى لفترة طويلة، فيجب عليك استشارة الطبيب بشأن العلاج بالليزر المتقدم. فهو بلا شك الخيار الأفضل للتعامل مع الحصوات التي تدمر حياتك.

كل ما تحتاج إلى معرفته حول جراحة زراعة القضيب
ما هي زراعة القضيب؟
يمكن أن يؤثر ضعف الانتصاب على أي رجل في أي عمر. هناك خيارات علاجية مختلفة مثل الأدوية والحبوب وعلاج التستوستيرون والحقن. لكن بعض هذه العلاجات قد لا تنجح مع بعض الرجال. قد يوصي بعض الأطباء بالحصول على غرسة القضيب. هناك نوعان من إجراءات غرس القضيب التي يمكن أن تساعد في حل مشاكل مختلفة. أحدهما قابل للنفخ والآخر غير قابل للنفخ. والغرض منه هو المساعدة في علاج ضعف الانتصاب ومع المتحولين جنسياً. في بعض الأحيان يتم استخدامه للمساعدة في إعادة بناء القضيب، إذا لزم الأمر. هنا، ستناقش Happy Urology جراحة غرسات القضيب، من كيفية عملها إلى تكلفة ذلك.
كيف تعمل عملية زرع القضيب؟
تعمل غرسات القضيب على المساعدة في الحفاظ على الانتصاب أو المساعدة في التأثيرات التجميلية. هناك نوعان رئيسيان هما الغرسات القابلة للنفخ وغير القابلة للنفخ. تتكون الغرسة القضيبية القابلة للنفخ من أسطوانتين ومضخة. يتم وضع الأسطوانتين في القضيب، والمضخة في كيس الصفن. لتحقيق الانتصاب، يقوم الشخص بالضغط على المضخة والأسطوانتين عن طريق ملئهما بمحلول ملحي. الغرسة غير القابلة للنفخ تحتوي على جراح يزرع قضيبين مرنين في القضيب. لا يتغير حجم القضبان أو صلابتها. تكون الغرسات دائمًا شبه صلبة، مما يجعل القضيب يشعر بنفس الشعور. لكن يمكن للأشخاص تحريكه إلى أي وضع يريدونه.
الحياة مع الغرسات؟
بعد العملية، يستغرق التعافي من جراحة زرع القضيب حوالي 4-6 أسابيع . يشعر الأشخاص الذين لديهم كلتا الغرستين بالرضا عن النتائج بعد العملية. يبلغ بعض الأشخاص عن عدم وجود أي فقدان للإحساس أثناء الجماع. لم يتأثر القذف بعد الجراحة. تترك الغرسة ندبة جراحية صغيرة لا يستطيع معظم الأشخاص رؤيتها. عند ارتداء الملابس، لا تكون الغرسات ملحوظة، لذلك يمكنك الشعور بالثقة في ارتداء الملابس التي تريدها. في معظم الحالات، يمكن أن تدوم الغرسة القضيبية ما بين 15 و20 عامًا.
كم تكلفة عملية الزرع؟
قد تصل تكلفة عملية زراعة القضيب إلى حوالي 14000 دولار أو أكثر. تغطي بعض شركات التأمين التكلفة إذا كانت العملية لعلاج ضعف الانتصاب. ومع ذلك، لا تغطي غالبية شركات التأمين الصحي عملية زراعة القضيب، وسوف يتحمل المريض تكاليفها. يقدم بعض الأطباء حزمة أسعار ويقدمون بعض الخصومات للمرضى.
معدل النجاح
لا تخلو أي عملية جراحية من المضاعفات، على الرغم من أن حوالي 90% من جراحات زراعة القضيب ناجحة. ولكن هناك بعض المخاطر.
- عدوى
- نسيج ندبي
- فشل المضخة
- عدم تصريف السائل بشكل صحيح
يمكن علاج أغلب المضاعفات بإجراء جراحة إضافية. لا تزال الغرسة عبارة عن جهاز ميكانيكي، لذا فهي معرضة لخطر الكسر. إذا حدثت أي مضاعفات، اتصل بطبيبك على الفور.
طب المسالك البولية السعيد
إذا كنت تعاني من ضعف الانتصاب وجربت العديد من خيارات العلاج المختلفة، فاتصل بمركز Happy Urology للحصول على استشارة أو لمعرفة المزيد عن جراحة زراعة القضيب. وسنساعدك في الإجابة عن أي أسئلة أو مخاوف بشأن زراعة القضيب أو أدوية ضعف الانتصاب. كما نقدم العديد من خدمات المسالك البولية المختلفة لتلبية احتياجاتك.
تبخير البروستات بالليزر الأخضر
لماذا يتم ذلك؟
تساعد جراحة البروستاتا بالليزر على تقليل الأعراض البولية الناتجة عن تضخم البروستاتا الحميد، بما في ذلك:
الحاجة المتكررة والملحة للتبول
صعوبة بدء التبول
التبول البطيء (المطول)
زيادة وتيرة التبول في الليل
التوقف والبدء مرة أخرى أثناء التبول
الشعور بعدم القدرة على إفراغ المثانة تمامًا
التهابات المسالك البولية
يمكن إجراء جراحة الليزر أيضًا لعلاج أو منع المضاعفات الناتجة عن انسداد تدفق البول، مثل:
التهابات المسالك البولية المتكررة
تلف الكلى أو المثانة
عدم القدرة على التحكم في التبول أو عدم القدرة على التبول على الإطلاق
حصوات المثانة
دم في البول
يمكن أن تقدم جراحة الليزر العديد من المزايا مقارنة بالطرق الأخرى لعلاج تضخم البروستاتا الحميد. قد يستغرق الأمر عدة أسابيع إلى أشهر لرؤية تحسن ملحوظ مع الأدوية.
التحسن في الأعراض البولية من جراحة الليزر ملحوظ على الفور. يمكن أن تشمل المزايا مقارنة بالجراحة التقليدية، مثل استئصال البروستاتا عبر مجرى البول واستئصال البروستاتا المفتوح، ما يلي:
انخفاض خطر النزيف.
يمكن أن تكون جراحة الليزر خيارًا جيدًا للرجال الذين يتناولون أدوية لتخفيف الدم أو الذين يعانون من اضطراب النزيف الذي لا يسمح لدمائهم بالتجلط بشكل طبيعي.
إقامة أقصر في المستشفى أو بدون إقامة.
يمكن إجراء جراحة الليزر على أساس العيادات الخارجية أو مع إقامة ليلة واحدة فقط في المستشفى.
التعافي بشكل أسرع.
يستغرق التعافي من جراحة الليزر عمومًا وقتًا أقل من التعافي من استئصال البروستاتا عبر مجرى البول أو الجراحة المفتوحة.
أقل حاجة إلى القسطرة.
تتطلب إجراءات علاج تضخم البروستاتا عمومًا استخدام أنبوب (قسطرة) لتصريف البول من المثانة بعد الجراحة. مع جراحة الليزر، تكون القسطرة مطلوبة عمومًا لمدة أقل من 24 ساعة.
تبخير البروستاتا بالريزوم الشرح الكامل للإجراء
ريزوم هو علاج طفيف التوغل لتضخم البروستاتا الحميد (BPH)، وهي حالة شائعة لدى الرجال المسنين حيث تتضخم البروستاتا وتؤثر على وظيفة التبول. يستخدم بخار الماء (البخار) لتقليل أنسجة البروستاتا. فيما يلي مزايا إجراء ريزوم:
1. طفيف التوغل
• يتم إجراؤه كإجراء خارجي، غالبًا دون الحاجة إلى تخدير عام.
• وقت تعافي قصير مقارنة بالخيارات الجراحية التقليدية مثل TURP (استئصال البروستاتا عبر مجرى البول).
2. يحافظ على الوظيفة الجنسية
• انخفاض خطر الآثار الجانبية مثل ضعف الانتصاب أو القذف الرجعي مقارنة بعلاجات تضخم البروستاتا الحميد الأخرى.
3. إجراء سريع
• يستغرق العلاج 10-15 دقيقة فقط، مما يجعله مناسبًا لكل من المرضى والمقدمين.
4. لا حاجة للأدوية طويلة الأمد
• يقلل الاعتماد على الأدوية اليومية لتضخم البروستاتا الحميد، والتي يمكن أن يكون لها آثار جانبية مثل الدوخة أو انخفاض الرغبة الجنسية.
5. تخفيف الأعراض بشكل فعال
• يشعر المرضى بتحسن كبير في أعراض المسالك البولية، بما في ذلك انخفاض وتيرة التبول والإلحاح والتبول الليلي (البوال الليلي).
6. نتائج دائمة
• تظهر الدراسات أن فوائد ريزوم يمكن أن تستمر لعدة سنوات.
7. انخفاض خطر المضاعفات
• انخفاض مخاطر النزيف الشديد أو العدوى مقارنة بالجراحات التقليدية.
8. تعدد الاستخدامات
• مناسب لمجموعة واسعة من أحجام وتكوينات البروستاتا.
9. الحد الأدنى من فترة النقاهة
• يمكن لمعظم المرضى استئناف الأنشطة الطبيعية في غضون أيام قليلة، مع بعض القيود المؤقتة على رفع الأشياء الثقيلة والأنشطة القوية.
10. مغطى بالتأمين
• تغطي العديد من خطط التأمين الصحي، بما في ذلك Medicare، إجراء ريزوم.
وعلى الرغم من هذه المزايا، فمن الضروري استشارة مقدم الرعاية الصحية لتحديد ما إذا كان ريزوم هو الخيار الصحيح، لأنه قد لا يكون مناسبًا للجميع، وخاصة أولئك الذين يعانون من أعراض شديدة أو غدة البروستاتا كبيرة جدًا.
شرح عملية الفيلر
هذه علاجات طفيفة التوغل تهدف إلى زيادة محيط القضيب. تتكون هذه الحشوات عادةً من مواد مثل حمض الهيالورونيك (HA)، وهي مادة متوافقة حيويًا تُستخدم أيضًا في حشوات الوجه. إليك نظرة عامة:
الإجراء:
1. الاستشارة: يقوم الطبيب بتقييم أهدافك وتشريحك وصحتك العامة لتحديد ما إذا كنت مرشحًا جيدًا.
2. اختيار الحشو: تُستخدم حشوات حمض الهيالورونيك عادةً لأنها مؤقتة وآمنة وقابلة للعكس.
3. التطبيق: يتم تطبيق التخدير الموضعي، ويتم حقن الحشو في الأنسجة تحت الجلد في عمود القضيب.
4. التعافي: فترة نقاهة ضئيلة، على الرغم من أنه قد يحدث تورم أو كدمات طفيفة. النتائج فورية.
الفوائد:
• إجراء سريع غير جراحي.
• يمكن عكسه باستخدام إنزيم (هيالورونيداز) إذا لزم الأمر.
• يمكن أن يحسن الثقة في المظهر.
المخاطر:
• كدمات أو تورم.
• ملمس غير منتظم أو عدم تناسق.
• نادرًا ما تحدث عدوى أو تفاعل تحسسي.
بالنسبة للخيارات الدائمة، قد يُقترح استخدام مواد مثل PMMA (بولي ميثيل ميثاكريلات) أو نقل الدهون جراحيًا. استشر دائمًا طبيب المسالك البولية المعتمد لاستكشاف الخيارات بأمان.

لماذا قد تكون زراعة القضيب هي الخيار الصحيح
مقدمة
يمكن أن يؤثر ضعف الانتصاب على أكثر من مجرد الصحة الجسدية، بل يمكن أن يؤثر على رفاهيتك العاطفية وعلاقاتك. بالنسبة للرجال الذين لم يجدوا النجاح مع العلاجات الأخرى، قد توفر زراعة القضيب فرصة جديدة للحياة. في هذا المنشور، نتعمق في الأسباب التي تجعل العديد من الأشخاص يختارون زراعة القضيب كجزء من رحلتهم لتحسين الصحة الجنسية.
استعادة الثقة واحترام الذات
يمكن أن يؤدي ضعف الانتصاب إلى الشعور بعدم الكفاءة أو فقدان الثقة. توفر زراعة القضيب حلاً موثوقًا به يساعد في استعادة الوظيفة الطبيعية للقضيب، مما يؤدي إلى تعزيز احترام الذات والشعور المتجدد بالرجولة.
مقارنة خيارات العلاج
• الأدوية الفموية مقابل الغرسات: في حين أن الأدوية مثل السيلدينافيل (الفياجرا) يمكن أن تكون فعالة للعديد من الأشخاص، إلا أنها ليست مناسبة دائمًا لكل مريض.
• الموثوقية طويلة الأمد: على عكس الحلول المؤقتة، توفر غرسات القضيب حلاً أكثر ديمومة، مما يمنح العديد من الرجال راحة البال ويقلل من قلق مشاكل الأداء.
تحسين رضا العلاقة
يجد العديد من الأزواج أن معالجة ضعف الانتصاب من خلال غرسة القضيب يمكن أن يحسن بشكل كبير العلاقة الحميمة والرضا العام عن العلاقة. يمكن أن تساعد المناقشات المفتوحة مع شريكك ومقدم الرعاية الصحية في تحديد التوقعات الواقعية وتعزيز الدعم المتبادل أثناء عملية التعافي والتكيف.
الخلاصة
يعد اختيار غرسة القضيب قرارًا شخصيًا للغاية - وهو القرار الذي يمكن أن يمكّنك من استعادة صحتك الجنسية وتحسين جودة حياتك بشكل عام. إذا كنت تستكشف خيارات العلاج الخاصة بك، ففكر في التحدث مع أخصائي لتحديد ما إذا كان هذا الحل الجراحي يتماشى مع أهدافك الصحية طويلة الأمد.
إخلاء المسؤولية: هذا المنشور للأغراض التعليمية فقط وليس بديلاً عن المشورة الطبية المهنية.

الدعامة الهيدروليكية
الدعامة الهيدروليكية: دليلك الشامل لعلاج ضعف الانتصاب في دبي
نحن ملتزمون بتقديم تجربة علاجية فريدة وراقية في دبي، تجمع بين الرعاية الطبية المتخصصة والخدمات السياحية الراقية. عند حجزك من خلال موقعنا، ستحصل على علاج متقدم في دولة الإمارات العربية المتحدة، مع تخطيط مسبق لرحلتك العلاجية والترفيهية.
مقدمة عن الدعامة الهيدروليكية
تُعد الدعامة الهيدروليكية حلاً ثورياً لعلاج حالات ضعف الانتصاب المزمن، خاصةً في الحالات التي لم تنجح فيها العلاجات الدوائية مثل الفياجرا. تتيح هذه التقنية تحكماً دقيقاً في الانتصاب من خلال نظام ضخ متطور، مما يجعلها الخيار الأمثل للرجال الذين يعانون من مشاكل صحية أو مضاعفات بعد الجراحات.
ما هي الدعامة الهيدروليكية؟
هي جهاز طبي يُزرع جراحياً داخل العضو الذكري، يعمل من خلال نظام هيدروليكي يضخ السوائل داخل أسطوانات مرنة لتحقيق انتصاب طبيعي وقابل للتحكم. وتتميز عن الدعامات الصلبة بمرونتها وإمكانية تفعيلها حسب الحاجة، مما يضمن راحة أكبر في الحياة اليومية.
المميزات الرئيسية:
-
تحكّم كامل في توقيت الانتصاب ومدته.
-
مظهر طبيعي في حالتي الارتخاء والانتصاب.
-
حل طويل الأمد (يدوم لسنوات) بنسبة نجاح تفوق %95
-
مناسبة لمرضى السكري، وإصابات الحوض، وضعف الانتصاب المزمن.
أنواع الدعامة الهيدروليكية
يتم اختيار النوع المناسب حسب احتياجات المريض وتوصيات الطبيب:
-
الدعامة ذات القطعتين:
-
تحتوي على مضخة وخزان مدمجين في وحدة واحدة.
-
تُزرع داخل العضو الذكري وكيس الصفن.
-
تتميز بسهولة التركيب وقلة التعقيد.
-
-
الدعامة ذات الثلاث قطع:
-
تتضمن مضخة منفصلة، وخزان سوائل يُزرع في البطن، وأنابيب مرنة.
-
توفر تحكماً أدق في صلابة الانتصاب ومظهراً أكثر طبيعية.
-
كيفية تركيب الدعامة الهيدروليكية
الخطوات الجراحية:
-
التخدير: عام أو نصفي.
-
الوصول إلى الأجسام الكهفية: عبر شق صغير في قاعدة العضو الذكري.
-
زراعة المكونات:
-
توضع الأسطوانات داخل الأجسام الكهفية.
-
تُثبت المضخة في كيس الصفن، والخزان (في حال الدعامة الثلاثية) في البطن.
-
-
الإغلاق: باستخدام غرز قابلة للامتصاص وضمادات معقمة.
مدة العملية:
من ساعة إلى ساعتين، مع إمكانية مغادرة المستشفى في نفس اليوم.
متى تُوصف الدعامة الهيدروليكية؟
-
عند فشل الأدوية أو العلاجات الطبيعية.
-
في حالات الضعف الناتج عن أمراض مزمنة كمرض السكري.
-
بعد جراحات السرطان أو الحوض.
-
لمن يبحث عن حل دائم دون الاعتماد على الأدوية.
إيجابيات وسلبيات الدعامة الهيدروليكية
| المميزات | العيوب |
|---|---|
| تحكم فوري في الانتصاب | تكلفة مرتفعة مقارنة بالدعامات المرنة |
| نتائج طويلة الأمد (10–15 سنة) | احتمال تسرب السوائل أو تلف المضخة |
| مناسبة للحالات المعقدة | مخاطر جراحية مثل العدوى أو النزيف |
نصائح ما قبل وبعد الجراحة
قبل العملية:
-
إجراء تحاليل وفحوصات الأشعة اللازمة.
-
التوقف عن التدخين ومضادات التخثر قبل أسبوع.
-
الصيام 6–8 ساعات قبل الجراحة.
بعد العملية:
-
تجنب النشاط البدني لمدة أسبوعين.
-
استخدام كمادات باردة لتخفيف التورم.
-
الامتناع عن العلاقة الحميمة لمدة 4–6 أسابيع.
-
متابعة الطبيب بانتظام.
الدعامة الهيدروليكية مقابل الدعامة المرنة
| الهيدروليكية | المرنة |
|---|---|
| تحكم كامل بالانتصاب | صلابة دائمة |
| مظهر طبيعي | تكلفة أقل |
| مناسبة للحالات الطبية المعقدة | حل بسيط وسريع |
الأسئلة الشائعة
هل تسبب الدعامة ألماً؟
قد يشعر المريض بألم خفيف بعد الجراحة، يزول باستخدام المسكنات.
متى يمكن العودة لممارسة الرياضة؟
بعد 4–6 أسابيع، حسب توصيات الطبيب.
هل تؤثر الدعامة على الإحساس أو القذف؟
لا، لا تؤثر على الوظائف الجنسية الطبيعية.
ختاماً
تقدم دبي تجربة علاجية استثنائية تمزج بين التكنولوجيا الطبية المتقدمة والرعاية الصحية المتكاملة. للاستفسار أو الحجز، تواصل معنا لنضع بين يديك خطة متكاملة لاستعادة الثقة والحيوية. 🌟

ضعف الانتصاب
ما هو ضعف الانتصاب؟
يُعد ضعف الانتصاب، أو ما يُعرف بـ ED، أكثر المشاكل الجنسية شيوعًا بين الرجال، حيث يُبلغ عنه الطبيب. ويُصيب ما يصل إلى 30 مليون رجل.
يُعرّف ضعف الانتصاب بأنه صعوبة في الحصول على انتصاب قوي بما يكفي لممارسة الجنس، أو الحفاظ عليه.
على الرغم من أنه ليس من النادر أن يُعاني الرجل من بعض مشاكل الانتصاب من وقت لآخر، إلا أن ضعف الانتصاب المُتفاقم أو الذي يحدث بشكل روتيني أثناء ممارسة الجنس ليس طبيعيًا، ويجب علاجه.
يمكن أن يحدث ضعف الانتصاب في الحالات التالية:
غالبًا عندما يكون تدفق الدم في القضيب محدودًا أو تتضرر الأعصاب.
بسبب التوتر أو لأسباب عاطفية.
كإنذار مُبكر لمرض أكثر خطورة، مثل: تصلب الشرايين (تصلب الشرايين أو انسدادها)، وأمراض القلب، وارتفاع ضغط الدم، أو ارتفاع نسبة السكر في الدم بسبب مرض السكري.
سيساعدك تحديد سبب (أسباب) ضعف الانتصاب في علاج المشكلة وتحسين صحتك العامة. كقاعدة عامة، ما هو مفيد لصحة قلبك مفيد لصحتك الجنسية.
كيف يعمل الانتصاب
أثناء الإثارة الجنسية، تُفرز الأعصاب مواد كيميائية تزيد من تدفق الدم إلى القضيب. يتدفق الدم إلى حجرتي الانتصاب في القضيب، المكونتين من نسيج عضلي إسفنجي (الجسم الكهفي). حجرتا الجسم الكهفي ليستا مجوفتين.
رسم تخطيطي لكيفية عمل الانتصاب
تكبير
أثناء الانتصاب، تسترخي الأنسجة الإسفنجية وتحبس الدم. ضغط الدم في الحجرتين يجعل القضيب مشدودًا، مما يُسبب الانتصاب. عندما يصل الرجل إلى النشوة الجنسية، تصل مجموعة ثانية من الإشارات العصبية إلى القضيب وتُسبب انقباض الأنسجة العضلية فيه، فيعود الدم إلى الدورة الدموية ويتراجع الانتصاب.
عندما لا تكون مُثارًا جنسيًا، يكون القضيب لينًا ومرنًا. قد يلاحظ الرجال أن حجم القضيب يختلف باختلاف الدفء أو البرودة أو القلق؛ وهذا أمر طبيعي ويعكس توازن الدم الداخل والخارج من القضيب. تم التحديث في يونيو ٢٠١٨
الأعراض
مع ضعف الانتصاب، يصعب الحصول على انتصاب قوي أو الحفاظ عليه بما يكفي لممارسة الجنس. عندما يصبح ضعف الانتصاب مشكلة روتينية ومزعجة، يمكن لمقدم الرعاية الصحية الأولية أو طبيب المسالك البولية مساعدتك.
قد يكون ضعف الانتصاب علامة تحذيرية رئيسية لأمراض القلب والأوعية الدموية، مما يشير إلى تراكم الانسدادات في الجهاز الوعائي للرجل. أظهرت بعض الدراسات أن الرجال الذين يعانون من ضعف الانتصاب معرضون بشكل كبير لخطر الإصابة بنوبة قلبية أو سكتة دماغية أو مشاكل في الدورة الدموية في الساقين. كما يُسبب ضعف الانتصاب ما يلي:
انخفاض تقدير الذات
الاكتئاب
الضيق للرجل وشريكته
إذا كان ضعف الانتصاب يؤثر على صحة الرجل أو علاقاته، فيجب علاجه. يهدف العلاج إلى إصلاح أو تحسين وظيفة الانتصاب، ودعم صحة الدورة الدموية، وتحسين جودة حياة الرجل.
تم التحديث في يونيو ٢٠١٨
الأسباب
يمكن أن ينتج ضعف الانتصاب عن مشاكل صحية، أو مشاكل عاطفية، أو كليهما. من عوامل الخطر المعروفة:
تجاوز سن الخمسين
ارتفاع سكر الدم (داء السكري)
ارتفاع ضغط الدم
الإصابة بأمراض القلب والأوعية الدموية
ارتفاع نسبة الكوليسترول
التدخين
تعاطي المخدرات أو الإفراط في شرب الكحول
السمنة
قلة ممارسة الرياضة
على الرغم من أن ضعف الانتصاب يزداد شيوعًا مع تقدم الرجال في السن، إلا أن التقدم في السن لا يُسببه دائمًا. يظل بعض الرجال قادرين على ممارسة الجنس حتى سن الثمانينيات. قد يكون ضعف الانتصاب علامة مبكرة على مشكلة صحية أكثر خطورة. يُعدّ اكتشاف سبب ضعف الانتصاب وعلاجه خطوة أولى حيوية.
الأسباب الجسدية لضعف الانتصاب
يحدث ضعف الانتصاب عندما:
لا يتدفق الدم الكافي إلى القضيب
يمكن للعديد من المشاكل الصحية أن تُقلل من تدفق الدم إلى القضيب، مثل تصلب الشرايين، وأمراض القلب، وارتفاع سكر الدم (داء السكري)، والتدخين.
لا يستطيع القضيب حبس الدم أثناء الانتصاب. إذا لم يبق الدم في القضيب، فلن يتمكن الرجل من الحفاظ على الانتصاب. يمكن أن تحدث هذه المشكلة في أي عمر.
لا تصل الإشارات العصبية من الدماغ أو النخاع الشوكي إلى القضيب.
قد تُلحق بعض الأمراض أو الإصابات أو العمليات الجراحية في منطقة الحوض الضرر بأعصاب القضيب.
قد يُسبب داء السكري أمراض الأوعية الدموية الدقيقة أو تلفًا في أعصاب القضيب.
قد تؤثر علاجات السرطان بالقرب من الحوض على وظيفة القضيب.
قد تُسبب الجراحة أو العلاج الإشعاعي لأورام سرطانية في أسفل البطن أو الحوض ضعف الانتصاب. غالبًا ما يُسبب علاج سرطان البروستاتا أو القولون والمستقيم أو المثانة ضعف الانتصاب لدى الرجال. ينبغي على الناجين من السرطان مراجعة طبيب المسالك البولية للاستفسار عن مشاكل الصحة الجنسية.
قد تؤثر الأدوية المُستخدمة لعلاج مشاكل صحية أخرى سلبًا على الانتصاب.
يجب على المرضى مُناقشة الآثار الجانبية للأدوية مع أطبائهم.
الأسباب العاطفية لضعف الانتصاب
يحتاج الجنس الطبيعي إلى تعاون العقل والجسم. قد تُسبب المشاكل العاطفية أو العاطفية ضعف الانتصاب أو تُفاقمه.
من بين المشاكل العاطفية التي قد تُسبب ضعف الانتصاب:
الاكتئاب
القلق
الخلافات في العلاقات
التوتر في المنزل أو العمل
التوتر الناتج عن الخلافات الاجتماعية أو الثقافية أو الدينية
القلق بشأن الأداء الجنسي
تم التحديث في يونيو ٢٠١٨
التشخيص
سيساعدك تحديد سبب ضعف الانتصاب على تحديد خيارات العلاج المُناسبة لك.
يبدأ تشخيص ضعف الانتصاب بسؤال مُقدم الرعاية الصحية عن صحة قلبك والأوعية الدموية ومشكلة الانتصاب. قد يُجري لك مُقدم الرعاية الصحية أيضًا فحصًا بدنيًا، أو يطلب فحوصات مخبرية، أو يُحيلك إلى طبيب مُسالك بولية.
التاريخ الصحي وضعف الانتصاب
سيطرح عليك طبيبك أسئلة

لماذا تختار د. خالد نذير الطبجي؟ ولماذا دبي هي الأفضل في العالم لهذا الإجراء؟
تُعد دبي اليوم واحدة من أفضل المدن عالميًا لإجراء زراعة دعامات القضيب الانتصابية، بفضل توفر الخبرات الطبية العالية، والبنية التحتية الصحية الحديثة، والمستشفيات المتقدمة التي تلتزم بأعلى معايير الجودة والأمان.
إضافةً إلى ذلك، تتميز دبي بسهولة السفر إليها من مختلف أنحاء العالم، وتوفر الخيارات السياحية الراقية التي تجعل رحلة العلاج تجربة مريحة وآمنة ومميزة.
أما د. خالد نذير الطبجي فهو من أبرز الجراحين المتخصصين في هذا المجال، بخبرة تمتد منذ عام 2010 في جراحة المسالك البولية والدعامات،
وحاصل على زمالة الجراحة البولية الأمريكية (2015)، والبوردين العربي والأردني، كما أنه خبير معتمد لشركة ZSI السويسرية ويمثل سوريا في مجال جراحة الدعامات منذ عام 2021.
يشتهر بدقته في التشخيص، وحرصه على راحة المريض، وفلسفته الطبية الواضحة:
“عدم إيذاء المريض، والتشخيص الدقيق قبل أي إجراء علاجي.”
💡 زراعة دعامات القضيب الانتصابية: خيار بسيط وآمن وفعّال
عندما تفشل الأدوية والعلاجات التقليدية في علاج ضعف الانتصاب، تكون زراعة الدعامة القضيبية هي الخيار الأمثل والأكثر نجاحًا.
وقد أثبتت الدراسات أن نسبة رضا المرضى تتجاوز 90%، خصوصًا مع استخدام الدعامات الهيدروليكية الحديثة ثلاثية الأجزاء.
🔹 خطوات التحضير والإجراء الجراحي
1. التقييم الطبي الكامل للحالة لمعرفة سبب ضعف الانتصاب واختيار النوع الأنسب من الدعامات.
2. التحضير قبل العملية ويشمل فحوصات عامة ومناقشة التوقعات والنتائج.
3. إجراء العملية تحت تخدير نصفي أو عام، وتستغرق عادة أقل من ساعة واحدة.
4. المتابعة بعد العملية تتم في نفس اليوم أو في اليوم التالي، مع تعليمات محددة للعناية.
5. العودة للنشاط الطبيعي تدريجيًا خلال 4 إلى 6 أسابيع، ويستعيد المريض الثقة الكاملة في الأداء الجنسي.
🏙️ لماذا تعتبر دبي الوجهة الأفضل لهذا النوع من الجراحة؟
• سهولة الوصول والسفر دون تعقيدات تأشيرة لمعظم الجنسيات.
• نظام صحي متطور وموثوق عالميًا.
• فنادق ومرافق تعافي راقية قريبة من المستشفيات.
• بيئة آمنة ومستقرة تجعل التجربة الطبية مريحة.
• إمكانية الجمع بين العلاج والسياحة في مدينة عالمية.
📊 الدراسات العلمية الداعمة
1. Çayan S, et al. Journal of Sexual Medicine. 2019;16(7):1092–1099.
2. Dadhich P, et al. Translational Andrology and Urology. 2017;6(5):885–893.
3. Moncada I, et al. International Journal of Impotence Research. 2025;37:61–65.
4. De Rocco Ponce M, et al. Journal of Clinical Medicine. 2025;14(14):5032.
🔸 الخلاصة
زراعة الدعامة القضيبية في دبي على يد د. خالد نذير الطبجي تمثل مزيجًا مثاليًا من الخبرة الجراحية، والأمان الطبي، والنتائج الممتازة.
إنها ليست مجرد عملية، بل خطوة لاستعادة الثقة والحياة الزوجية بشكل طبيعي وآمن.
تم إعداد هذا المقال لأغراض التثقيف الطبي العام بإشراف د. خالد نذير الطبجي.
آخر الأخبار
-

-

ضعف الانتصاب
23 July -

الدعامة الهيدروليكية
13 April
